PERIPHERAL AVM EMBOLIZATION
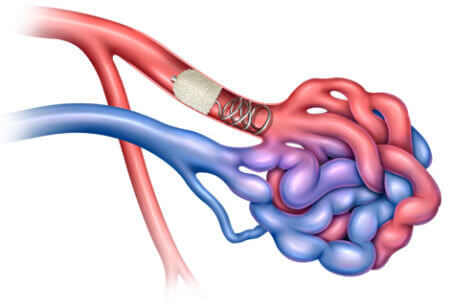
A peripheral arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the normal capillary network. This can occur in various parts of the body, most commonly in the arms and legs. Peripheral AVM embolization is a minimally invasive procedure used to close off these abnormal connections.
Understanding Peripheral AVMs:
- Arteries carry oxygen-rich blood away from the heart.
- Veins carry oxygen-depleted blood back to the heart.
- Capillaries are tiny blood vessels where oxygen and nutrients are exchanged with tissues.
In an AVM, arteries connect directly to veins, bypassing the capillaries. This can cause various problems, including:
- Enlarged, varicose veins
- Pain
- Swelling
- Skin ulcers
- High-output heart failure (rare)
Peripheral AVM Embolization Procedure:
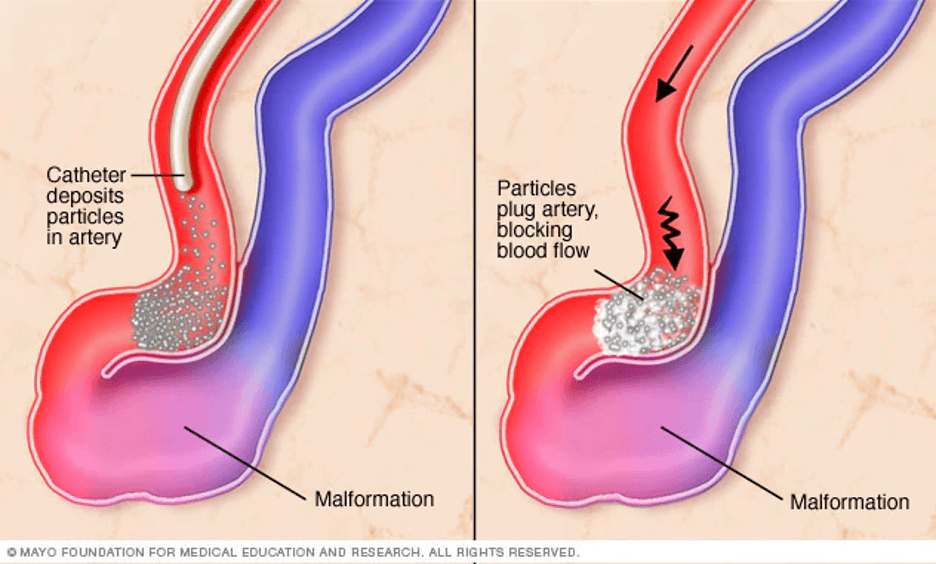
Embolization is a technique that uses a catheter to deliver a blocking material (embolic agent) to the AVM. Here’s a breakdown of the process:
- Access: A thin, flexible tube (catheter) is inserted into an artery in the groin or arm and guided through the blood vessels to the feeding artery of the AVM.
- Embolic Agent Delivery: Different types of embolic agents can be used, such as:
- Coils: Tiny, spring-like devices that block blood flow.
- Glues: Liquid agents that harden and block the connection.
- Particles: Small spheres that block smaller vessels within the AVM.
- Occlusion: The embolic agent is deployed, blocking the abnormal connection between the artery and vein.
- Closure: The catheter is removed, and the access point is closed.
Benefits of Embolization:
- Minimally invasive compared to surgery.
- Effective in treating many AVMs.
- Offers faster recovery time.
- Can be performed in stages for complex AVMs.
IR (Interventional Radiology) Treatment:
Embolization is performed by an interventional radiologist (IR) using fluoroscopy (live X-ray) guidance. IRs use image-guided minimally invasive procedures to diagnose and treat various conditions. Their expertise in navigating catheters within the vascular system makes them well-suited for embolization procedures.
Pre-procedural Workup:
Before embolization, a thorough evaluation is crucial. This may involve:
- Imaging studies: Angiography (X-ray of blood vessels) with contrast dye is essential to map the AVM’s anatomy, including feeding arteries, draining veins, and the nidus (central tangle of vessels). Ultrasound and MRI may also be used for additional information.
- Physical examination: Assessing symptoms like swelling, pain, and skin changes helps determine the severity of the AVM.
Types of Embolic Agents:
The choice of embolic agent depends on the specific AVM characteristics:
- Coils: Ideal for larger feeding arteries and the nidus. They come in various shapes and sizes for optimal placement.
- Liquid embolic agents: These include glues (e.g., n-butyl cyanoacrylate) and Onyx (ethylene-vinyl alcohol copolymer). They are useful for smaller vessels and can conform to complex shapes within the AVM.
- Sclerosing agents: These, like absolute ethanol, irritate the vessel lining, causing controlled clotting and closure.
- Embolization particles: Tiny spheres or plugs used to block smaller connections within the AVM.
Procedural Variations:
- Transarterial Embolization: The most common approach, accessing the AVM via the feeding arteries.
- Transvenous Embolization: Used in specific cases where accessing the arteries is difficult. It involves entering the draining veins and navigating upstream to block the connection.
- Combined Approach: Sometimes, both arterial and venous access are used for complex AVMs.
Post-procedural Care:
- Monitoring for bleeding, infection, and any worsening of symptoms.
- Repeat imaging to assess the success of embolization and identify any residual connections.
- Compression stockings may be recommended to improve circulation and reduce swelling.
- Depending on the complexity, additional embolization sessions might be needed.
IR Expertise in Embolization:
Interventional radiologists (IRs) possess unique skills for embolization:
- Vascular Anatomy Knowledge: Their in-depth understanding of blood vessel anatomy allows them to navigate the catheter precisely within the vascular system.
- Image-Guided Techniques: IRs use fluoroscopy (live X-ray) to visualize the catheter’s position and ensure accurate placement of the embolic agent.
- Minimally Invasive Approach: Embolization offers a less invasive alternative to open surgery, minimizing patient discomfort and recovery time.
Emerging Techniques:
The field of interventional radiology is constantly evolving. Here are some promising advancements:
- Microcatheters: These allow access to even smaller vessels within the AVM, improving treatment accuracy.
- 3D Imaging Integration: Advanced imaging techniques like 3D rotational angiography can provide a more detailed view of the AVM, aiding in treatment planning and navigation.
- Newer Embolic Materials: Research into biocompatible and biodegradable embolic agents is ongoing, offering potential advantages for long-term outcomes.
Conclusion:
Peripheral AVM embolization is a valuable tool in the interventional radiologist’s arsenal for managing these vascular malformations. By understanding the procedure, the role of IRs, and the latest advancements, we can ensure optimal treatment for patients with peripheral AVMs.











