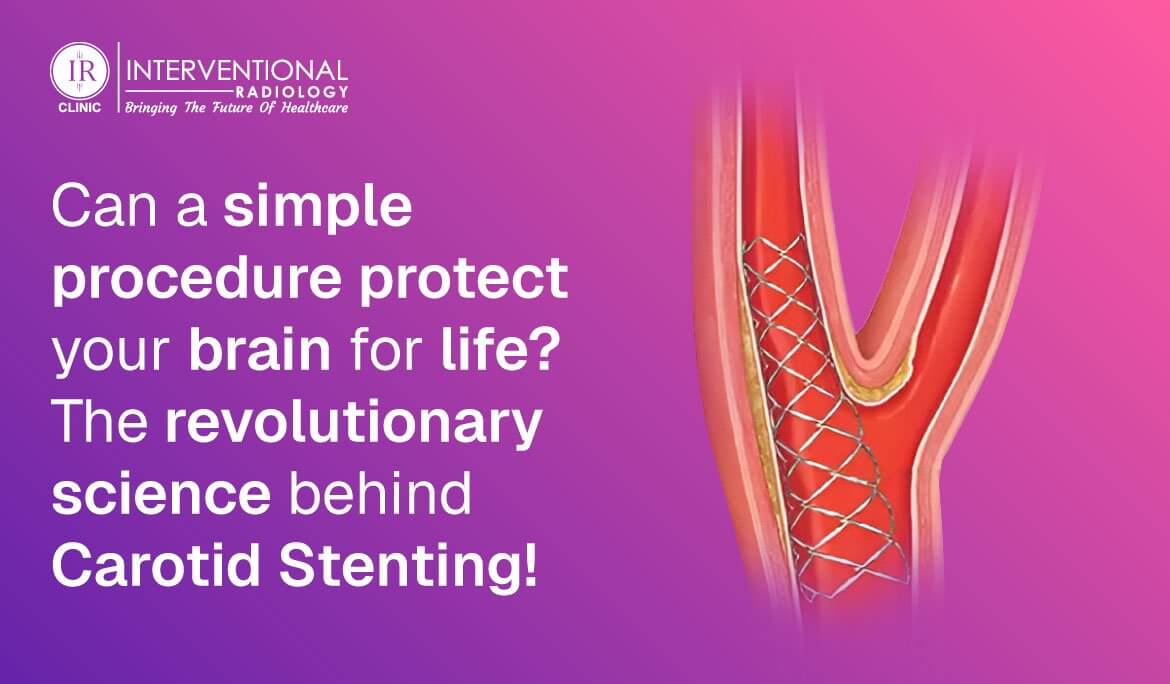
Carotid stenting has become a key intervention in stroke prevention, providing a less invasive option to the older surgical techniques such as carotid endarterectomy (CEA). New developments in interventional radiology (IR) have greatly improved the safety and effectiveness of carotid stenting, with it becoming a highly sought-after treatment for high-risk carotid stenosis. This post explores the current innovations in carotid stenting, such as drug-eluting stents and embolic protection devices, and the takeaways from seminal trials such as the CREST study.
Recent Innovations in Carotid Stenting
Drug-Eluting Carotid Stents:
These stents release medication that inhibits the formation of new tissue, minimizing the risk of restenosis. Although drug-eluting stents are more frequently linked with coronary interventions, studies on their use in carotid stenting are underway, with the potential for better outcomes through reduced need for repeat procedures.
Embolic Protection Devices (EPDs):
EPDs have changed the game of carotid stenting by catching debris in the process, and thus minimizing the risk of stroke. EPDs have played an important role in enhancing the safety profile of carotid stenting to make it a more feasible treatment for high-risk stenosis.
Bioresorbable Carotid Stents:
The carotid stent of the future could be bioresorbable stents, which slowly disintegrate in the course of time, potentially eliminating long-term complications from permanent stents. While still in the experimental stages, these stents are an exciting direction for future carotid stent technology.
CREST Trial Results and Carotid Stenting
The Carotid Revascularization Endarterectomy Versus Stent Trial (CREST) was a seminal trial comparing carotid stenting and CEA in symptomatic and asymptomatic patients. The trial concluded that the two procedures had comparable short- and long-term results, with a minor stenting advantage in younger patients and surgery in older patients24. The CREST-2 trial extends this investigation, comparing intensive medical management with and without stenting or endarterectomy, reflecting the changing knowledge of these procedures.
Interventional Radiology to Prevent Stroke
Interventional radiology is instrumental in stroke prevention through its ability to provide minimally invasive procedures such as carotid stenting. The advantages of IR are a shorter recovery time, decreased chances of complications over open surgery, and the capacity to treat patients who might not be suitable candidates for surgery based on comorbid conditions.
Guidelines on Carotid Stenting 2025
As we enter 2025, carotid stenting guidelines will probably reinforce the need for patient selection, operator expertise, and the utilization of sophisticated technologies like EPDs. Best practices will involve complete pre-procedure assessment, ideal antiplatelet therapy after stenting, and continuous monitoring to achieve the optimal results.
Future Directions and Innovations
Telemedicine After Carotid Stenting: Telemedicine integration can improve post-procedure management through remote monitoring and follow-up, enhance patient compliance, and lower healthcare expenditures.
Gene-Eluting Stents Research:
Ongoing research on gene-eluting stents may provide novel means of preventing restenosis and enhancing long-term results.
Case Series and Clinical Data:
Ongoing clinical trials and case series will continue to narrow our knowledge of carotid stenting, giving important information about its safety and efficacy in a wide variety of patient groups.
In summary, the practice of carotid stenting continues to progress dynamically, propelled by advances in interventional radiology and novel technology. In looking ahead, incorporating next-generation stents, protective devices, and telemedicine will revolutionize strategies for preventing strokes, providing more effective and less risky options for patients.